|
||||
| The Angio Institute | Research & Education | Brain Health Program | AngioNews/Media | Joining Hands |
Earlier Detection According to the American Cancer Society, women ages 45 to 54 and post-menopausal years are required to get mammograms every year. But for the underserved ages (20-39), the risk for breast cancer exists in growing numbers and it is just as real in growing numbers. The ANGIOFOUNDATION and the INTEGRATIVE WOMEN’S HEALTH ALLIANCE joined to develop and promote this national screening & advocacy program for women of younger age groups. A major concern is the presence of breast cancer in underserved communities, including those TOO YOUNG FOR A MAMMOGRAM. Decades into the battle against breast cancer, clinicians and the public are much more educated about EARLY DETECTION, PREVENTION and the current protocols and modalities available to save lives. Recent headlines on DENSE BREAST and the advancements in ULTRASOUND SCANNING supports a major part of this battle.
TURNKEY PROGRAM: EDUCATION & CLINICAL ACTION PLAN FOR EARLIER DETECTION
The AngioFoundation promotes addressing the continuing concerns for breast cancer by partnering with local imaging facilities, OBGYN practices and women's centers. We offer the installation of early detection screening starting with a comprehensive training program about medical breast imaging. This includes practical training of 3D Ultrasound technology to detect abnormalities in the breast. In addition. Active women's health practices may also qualify for grants and funding to support the promotion of early detection in our targeted "GEN-Z community" as part of public awareness and advocacy for women's health.
If your practice is interested in promoting EARLIER DETECTION, our turnkey program can help you get started right away. Contact the AngioFoundation programming dept at: 212.355-7017 Breast Density 101
Drastic changes in the incidence, diagnosis and treatment of breast cancer and benign breast disease highlight a singular need for an up to date source on the early detection and proper therapy of breast tumors. The age of occurrence of breast cancer, formerly only a problem of older women, is now at a median age of 45 years. This means that women in their twenties are developing breast cancer. Although risk factors have been identified, the jeopardy to life is unchanged. The increasing use of estrogen for osteoporosis and other female disorders may elevate the risk of breast cancer. One out of every eight women will develop breast cancer. Fortunately, the vast majority of tumors in younger women are benign and can be diagnosed by simple, safe non surgical tests. Jewish women, prone to breast cancer, are further plagued by the concomitant presence of fibrocystic breasts that are lumpy and mask a growing breast cancer. The incidence of miss by mammography increases markedly in younger patients and those with "mastitis" or "cystic" breasts. A paper from the University of Indiana Medical Center on the mammographic diagnosis of fibroadenomas (benign tumor of young women) demonstrated that in 35 surgically proven biopsies, the mammogram missed every mass. A non x ray exam, called the sonogram, was able to diagnose every tumor in this study. Another non-x ray test, called Doppler ultrasound, according to DIAGNOSTIC IMAGING (1988) and CLINICAL RADIOLOGY (1990) may detect breast tumors not seen by all other tests. Light scanning is another procedure that uses computers and fiberoptics to visualize tumors. The latest text book on Breast Disease, BREAST ULTRASOUND by Thomas Stavros (Lippincott, 2002) mentioned that most abnormalities of the breast may be better characterized or even detected only by diagnostic ultrasound procedures. JAMA (May 1993) noted mammography readings were highly variable with many false positives. Moreover, one expert missed 67% of cancers on high quality mammograms. Indeed, top mammographers disagreed clinically in 1/3 of readings. Since cancers may lie dormant for up to ten years and that mammography is less accurate in younger women, one realizes that sonography becomes necessary for a complete workup in the detection of invasive. Mayo Clinic computer program shows sonograms capable of 99% accuracy. The latest malpractice newsletters warn physicians that they are liable if they miss a breast cancer because they have not performed a sonogram. In fact, the PIAA Data Sharing Report shows that the patient found the tumor in 69% of cases, mammography missed or was equivocal in 49% and the median age of breast cancer was 43 years of age. False negatives were highest in the under age 40 group comprising 40% of claims.
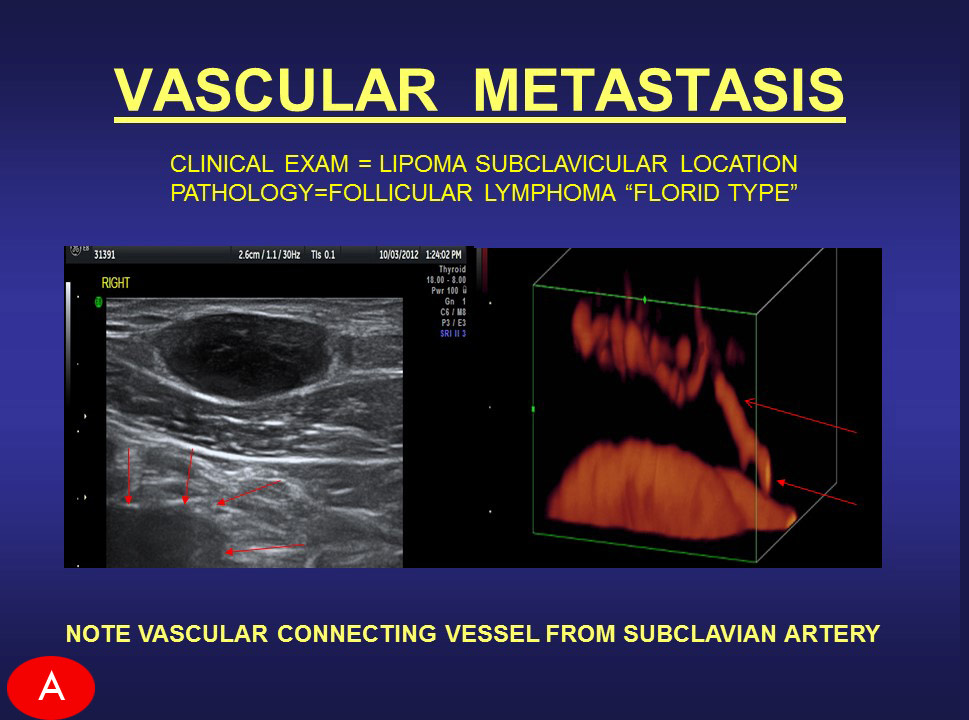
Pathological Views of DENSE BREAST TISSUE There is a significant correlation between AGE and BREAST TISSUE DENSITY Decades since the advent of breast scanning technology, innovations in non-invasive diagnostic imaging provide new options in the field of early detection. A mammogram can show how dense your breasts are including how low or high in density. However, over-compression artificially lowers the radiographic density. [Image 1] in this standard mammogram, a dense breast is presented side by side. The white shaped “V” that comes down the top center are the pectoral muscles of the chest wall. On the far outside, the white line is the skin outline of the breast. This is the dermal tissue causing the white line viewed enface. Radiologists always study this for any indication of inflammatory disease of the skin or inflammatory breast cancer, which manifests itself in skin thickening. Between the center wedge and the skin outline, you will find homogeneous cloudy areas with patchy black spaces within as an example of dense breast tissue.
Usually, dense breast tissue appears white on a mammogram. We must identify them as one of two forms of breast density; one is called FIBROCYSTIC or fibrous [Image 2] which is homogeneously white. Occasionally you can see a branching of blood vessels, dilated ducts or a streak of fat inside the dense breast tissue. This is the most common type of dense breast tissue and generally seen in the over 40 population. [Image 3] Another example of a dense breast shows the difference between homogeneous white versus the whitish area. This is filled with dark, wormy looking structures, which are the breast glands called GLANDULAR tissue. This kind secretes milk and its glands are often dilated. Both Fibrous and Glandular may appear similar under a mammogram as highly dense areas, but they look completely different under an ultrasound scan. Through ultrasound, we can check for tumors easily through fibrotic dense breasts because it stands out as a black region (or a black hole) within the white area. As shown in Image 3, a black hole could get lost, making it more difficult to image this type of dense breast. In this case, a solution is the use of elastography [Image 4], which offers visual confirmation as indicated by color data. Elastography can measure tissue density (its hardness or elasticity) within the glandular breast tissue. This tissue type is more common in the under-40 age group and is associated with other glandular proliferation such as endometriosis and is reportedly linked to dermal inflammation. In published reports, comparative studies between FIBROUS and GLANDULAR breast tissue studies remain limited. We are observing (especially in the younger age groups) expanding reviews of these types of tissue density aligned with the rates of breast cancer to confirm the rate of malignancy in tissue alteration from normal.
|
|||||||||||||
| DEDICATED MONITORING OF PRE AND POST-TREATMENT PROGRESS Within a closed testing program of 45-50 patients, a comparative review of pre and post treatment allows the developer a clear view of its efficacy and performance. Through the use of various imaging technologies and the experienced assessment strategies of our diagnosticians, we are able to provide the desired data which leads the devleoper to identify quality standards as they apply to the inevitable end user en masse. |
Educational PROGRAMS
The AngioFoundation has been recognized worldwide by official medical organizations and peer reviews for its work in FIVE MAIN focal topics and class divisions. We continually maintain and update research works in these categories to support the advancement of these disciplines as part of The AngioFoundation's commitment to the scientific community.
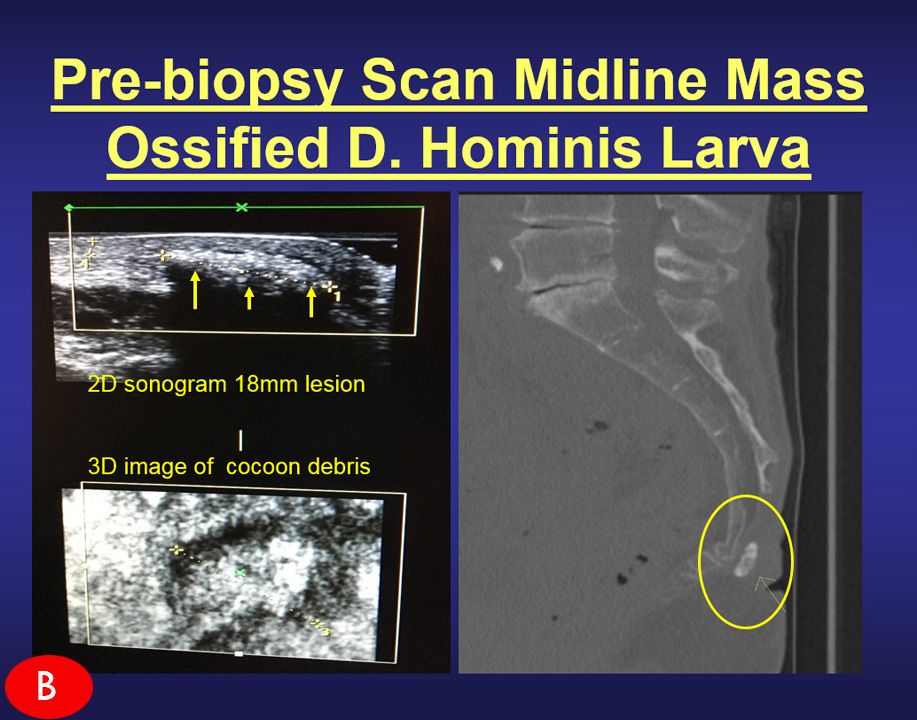
 Advanced use of Doppler Sonographic Imaging technology to identify malignant cancers and monitor their behavior through blood flow parameters- (Breast, Lung, Bladder, Prostate, Melanoma, etc) which correlates with comparative studies with other current technologies such as MRI, CT etc. Advanced use of Doppler Sonographic Imaging technology to identify malignant cancers and monitor their behavior through blood flow parameters- (Breast, Lung, Bladder, Prostate, Melanoma, etc) which correlates with comparative studies with other current technologies such as MRI, CT etc. |
 Research / assessment of musculoskeletal disorders (arthritis, inflammation, trauma) and dermatological issues through the advanced use of 3D/4D ULTRASOUND innovations. Research / assessment of musculoskeletal disorders (arthritis, inflammation, trauma) and dermatological issues through the advanced use of 3D/4D ULTRASOUND innovations. |
 TECH REVIEWER: Beta-testing, industry-wide comparative feature review/evaluation program. Drafting of FDA application / compliance documentation of digital imaging technologies (models, brands and generations) including sub-dermal and musculoskeletal treatment devices TECH REVIEWER: Beta-testing, industry-wide comparative feature review/evaluation program. Drafting of FDA application / compliance documentation of digital imaging technologies (models, brands and generations) including sub-dermal and musculoskeletal treatment devices |
 Internal study of all cancer issues and health disorders of victims associated with 9/11 and other disaster-related environmental toxic exposures. Collaboration with geological labs & environmental statistics. (See First Responders Cancer Resource) Internal study of all cancer issues and health disorders of victims associated with 9/11 and other disaster-related environmental toxic exposures. Collaboration with geological labs & environmental statistics. (See First Responders Cancer Resource) |
 Function review / performance evaluation program of all laser-based medical equipment including devices specializing in sub-dermal musculatory treatment of chronic disorders. Function review / performance evaluation program of all laser-based medical equipment including devices specializing in sub-dermal musculatory treatment of chronic disorders. |