Advantages of 3D Imaging in Burn Diagnostics & Foreign Body Scans
 |
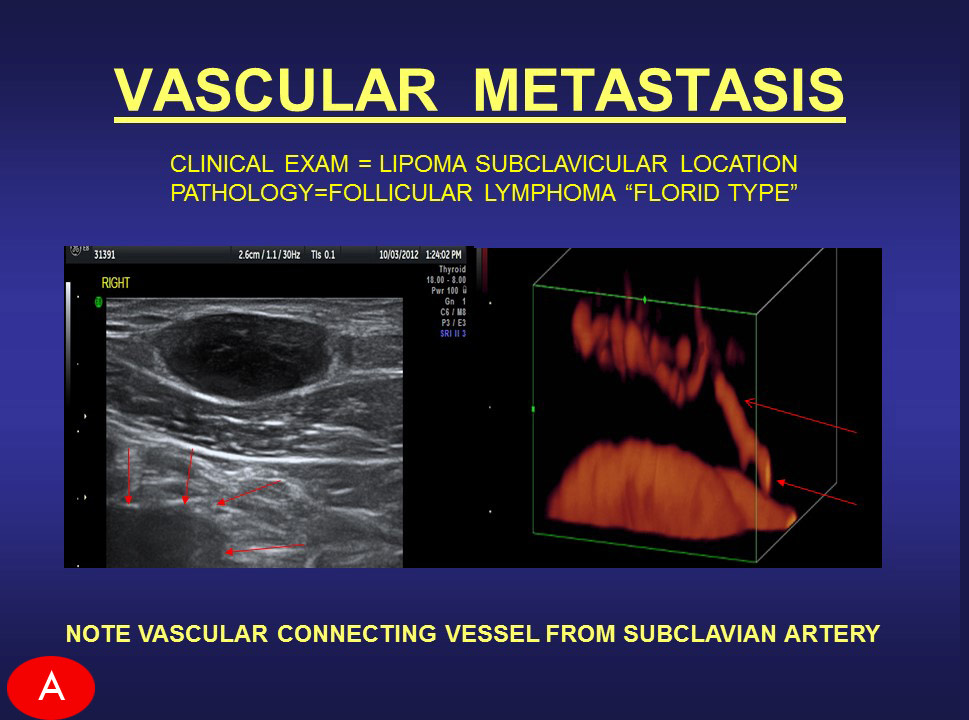
Today's advancements in imaging technology allows for REAL-TIME scanning power. By this, the provider can acquire more inforamtion about the existing trauma on or underneath the skin of the patient thanks to its advanced flexibility, performance and operational range. Real-Time scanning brings navigation power to the diagnosing of any subject by allowing the operator to manually aim the probe in any position or direction to 'shoot' unlimited angles of the target zone. This ability also greatly enables the manual steering of the probe while searching for things like moving tumors and foreign bodies like splinters and shattered glass particles. Unlike the still-image scanning concept of an MRI (where each click of the camera is one still photo), real-time scanning performs more like a video camera (shooting 30 frames/second) allowing a true action scan power for faster searching, identifying, monitoring and tracking- giving complete targeting control at the hand of the operator. Another major benefit to using real-time imaging is the introduction of data access from the ability to read any abnormalities of vascular flow.
|
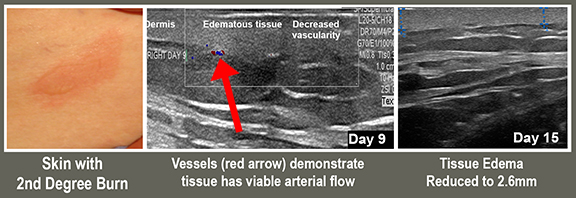
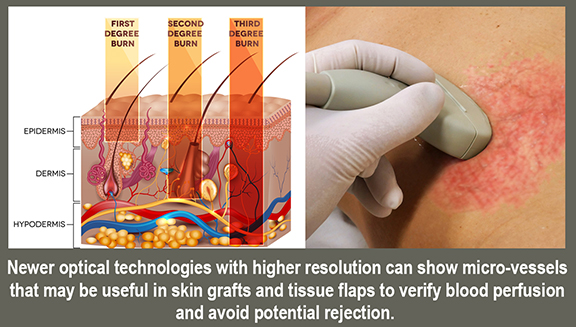
All major skin injuries relating to acute wounds and burns requires a better way to evaluate trauma depth and wound healing without the risk of complications. The application of high-frequency sound waves allows us to identify and analyze dermal and subdermal injuries. Imaging such as the high resolution 3D sonograms / Doppler technology brought a new wave of efficiency, safety and performance when it comes to assessing physical trauma, thus adding accuracy and confidence in the treatment process. Where NON-INVASIVE and NON-RADIATION technologies can provide safe, accurate readings and real-time tracking to any dermal trauma, modern imaging is especially useful and effective in cases like identifying foreign bodies on and under the skin. This ensures much less risk for complications or potential hazards during the diagnostic evaluation or pre-op stage (as opposed to skin sampling or biopsies)- especially in the case of studying the intensity of burns and depth during on-site diagnoses. From the establishment of DEPTH OF INJURY (or burn depth) and the VIABILITY OF THE TISSUE, the use of ultra-high resolution sonography (UHR) analyzes oxygenation and vascularity and oxygenation of the tissue. Other technologies that carry similar scanning advantages include:
• Near Infrared Spectroscopy (NIS)
• Thermography
• Nuclear Radiotracer Analysis
• Fluorescent imaging
• Hyperspectral imaging
• Laser Doppler imaging (LDI)
• Multiphoton microscopy
• Reflectance confocal microscopy (RCM)
• Optical coherence tomography
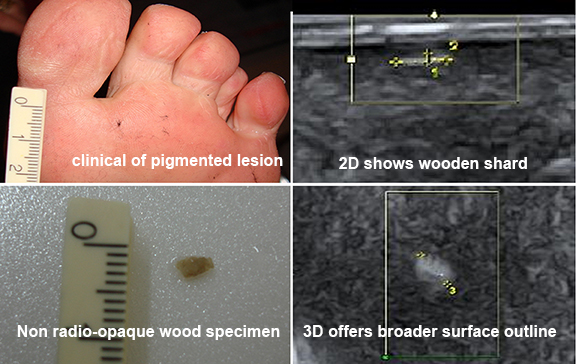 |
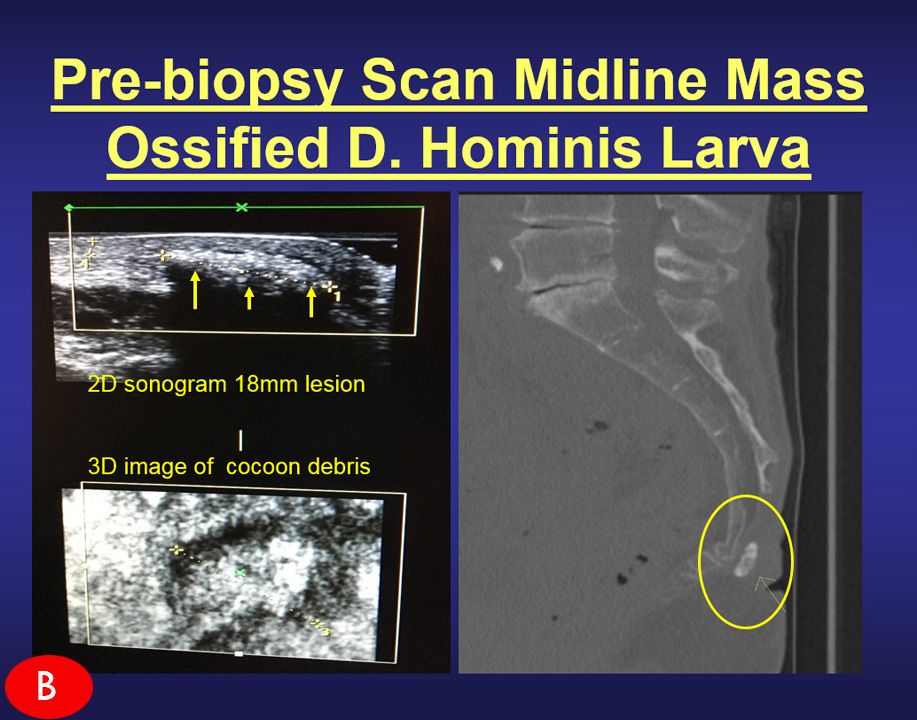
TARGETING FOREIGN BODIES
Where 2D imaging falls short in performance, the use of sonography is particularly important in finding and tracking foreign bodies. These are weight bearing anomalies that indicate movement in the penetrated tissues. Elements like fibers, metals or glass may leave fragments and splinters under the skin and can travel in unexpected locations beyond the area of entry.
Finding these foreign bodies within the horizontal plane becomes a more efficient process from the use of 3D sonography because imaging (here) is no longer limited to scanning from a single flat plane of a still image, but 3D and 4D potential adds singificant advantage in the scan and search process by allowing the operator to perform real-time adjustment (nagivation of probe) including angling & positioning to optimize the very movement of the foreign body where they may hide.
Additional TRAUMA related options where high resolution 3D Ultrasound technologies have offered similar advantages include: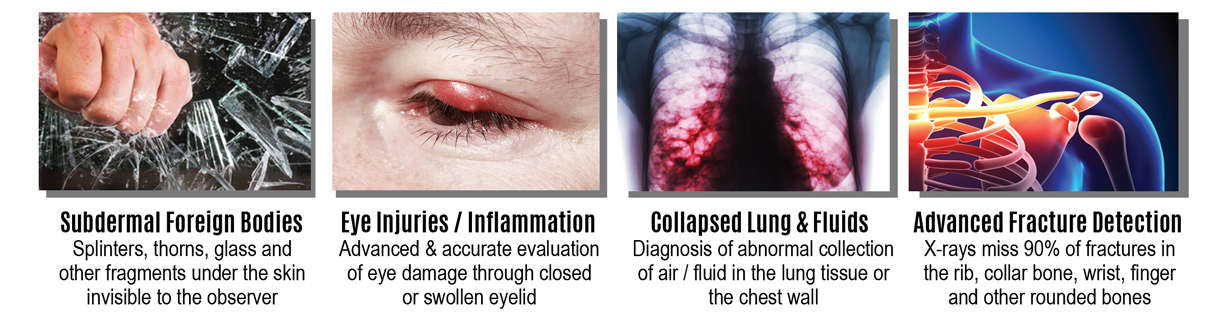

HHS sponsors development of portable, user-friendly burn imaging device
 |
Program advances next-generation technology to improve care for burn patients
July 18, 2019- An imaging device to evaluate the severity of burn injuries quickly and accurately will take the next steps in development under a contract by U.S. Department of Health and Human Services’ Office of the Assistant Secretary for Preparedness and Response (ASPR). Fast, accurate information about burn severity is critical to provide the appropriate care for patients. This enhanced triage ability will be particularly important in any type of mass casualty incident involving burns, including those resulting from a nuclear detonation. Triaging and treating burns effectively requires early clinical evaluations on the depth and severity of the injury. This initial clinical assessment informs a healthcare provider whether surgical procedures are necessary or if wounds will heal with other non-surgical treatment. (See complete press release @ PHE.gov)
..................................................................................................................................................................................................................
THERMOGRAPHY to assess burn wound healing potential: a reliable and valid technique when compared to laser Doppler imaging
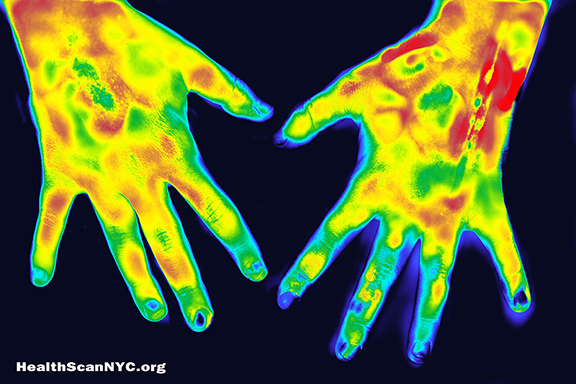 |
Adequate assessment of burn wound healing potential (HP) is crucial in the management of burn patients. Clinical (subjective) evaluation is the most widely used method for determining the expected burn wound outcome. This type of assessment is based on the probability of whether a wound will heal spontaneously (<3 weeks) or requires surgical therapy. This distinction in healing time is made, as wounds with a low HP (>3 weeks) are correlated with a significantly lower scar quality.1,2 Thus, underestimation of the healing time may lead to an increased risk of pathological scar formation, whereas overestimation of the healing time may increase the amount of needless surgery. It is easy to identify the mild injury of sunburn or to discern the other extreme: a dry, inelastic, insensitive, cadaveric-appearing wound that reflects serious injury to the skin. However, when a burn wound is first evaluated it is often difficult to determine the subtle differences and its potential to heal. Accordingly, clinical evaluation is not always sufficient as it is accurate in only 70% of the cases.3 This accuracy is even lower for inexperienced surgeons, around 50%.4,5 Therefore, objective tools that improve the assessment of burn wound HP are of great relevance. (see complete article)
Original Source: The SPIE DIGITAL LIBRARY / Authors:Mariëlle E. H. Jaspers M.D.,Ilse Maltha, John H. G. M. Klaessens, Henrica C. W. de Vet, Rudolf M. Verdaasdonk, Paul P. M. van Zuijlen M.D. /13 September 2016 / Creative Commons 4.0 license
..................................................................................................................................................................................................................
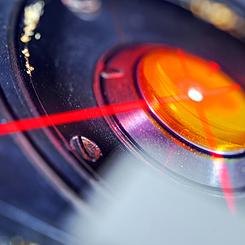
Cost-effectiveness of LASER DOPPLER IMAGING in burn care in the Netherlands
| photo |
Overestimation of burn depth can lead to unnecessary excision and grafting [2, 3]. On the other hand, underestimation of burn depth may lead to an unnecessary delay in surgery, with a longer length of hospital stay and higher hospital costs as a consequence [4, 5]. In burn care, traditionally classified as expensive care, there is a growing interest in costs and cost control [6, 7]. In order to provide effective and cost-effective burn care, there is a need for an accurate method for burn depth estimation.
Laser Doppler imaging (LDI) is the only technique that has been shown to accurately predict wound depth with a large weight of evidence. Laser Doppler imaging is based on the Doppler principle. Laser light that is directed at moving blood cells in sampled tissue exhibits a frequency change that is proportional to the amount of perfusion in the tissue. Laser Doppler imaging combines the advantages of laser Doppler and scanning techniques: the whole burn can be sampled and no direct contact with the burn surface is necessary. In daily practice, LDI will be used in combination with standard clinical assessment, as a so-called add-on test. (see complete article)
Original Source: BMC PART OF SPRINGER NATURE / . /1 February 2013 / Creative Commons 4.0 license
 |
Health & Safety PROGRAMS
The AngioFoundation is committed to philanthropic efforts and health/safety services pertaining to ALL CANCER ALERTS in our community.We are founded on the principles of front-line response to environmental emergencies, health epidemics and product hazards and recalls that affect a widespread group of victims. We support the community at large through the following key programs:
• PUBLIC ACCESS TO ADVANCED CANCER SCREENING & DIAGNOSTICS
• FUNDRAISING FOR CLINICAL RESEARCH, TRIALS & SCREENINGS & SCREENINGS
• CANCER EDUCATION, PUBLIC OUTREACH & AWARENESS PROJECTS
• SCHOLARSHIPS, GRANTS & DONOR CONTRIBUTIONS
• CAREGIVER NETWORK SUPPORT FOR PROFESSIONALS MANAGING CHRONIC DISORDERS
|
"GET CHECKED NOW!" and the
Public Access Program for Advanced Cancer Screening & Diagnostics (CSDS)
For New York residents who are having financial difficulties affording a second opinion outside of their current healthcare plan- or show income restrictions to pay out of pocket for advanced imaging or cancer diagnostic services, you may qualify for THE ANGIOFOUNDATION CSDS grant. The AngioFoundation partners with other cancer funding sources and research groups to bring full or partial financial aid to cancer-related emergencies. Our outreach program conducts outreach efforts and helps to complete the application process toward receiving screening & cancer scanning care. The "GET CHECKED NOW!" project was established in 2017 by the founders of NYCRA (The NY Cancer Resource Alliance) and was originally launched as a public awareness mission to bring vigilance and proactive attention to getting regular health checkups. This mission promotes early detection and prevention of cancer by raising the level of public health priority by identifying the many forms of cancer plaguing our society today.
"Get Checked Now!" also stays current with all public emergencies, occupational hazards, geographic carcinogens, medical recalls and other widespread health concerns.
Research & Educational PROGRAMS
The AngioFoundation has been recognized worldwide by official medical organizations and peer reviews for its work in FIVE MAIN focal topics and class divisions. We continually maintain and update research works in these categories to support the advancement of these disciplines as part of The AngioFoundation's commitment to the scientific community.
 Advanced use of Doppler Sonographic Imaging technology to identify malignant cancers and monitor their behavior through blood flow parameters- (Breast, Lung, Bladder, Prostate, Melanoma, etc) which correlates with comparative studies with other current technologies such as MRI, CT etc. (See cancerscan.com) Advanced use of Doppler Sonographic Imaging technology to identify malignant cancers and monitor their behavior through blood flow parameters- (Breast, Lung, Bladder, Prostate, Melanoma, etc) which correlates with comparative studies with other current technologies such as MRI, CT etc. (See cancerscan.com) |
 Research / assessment of musculoskeletal disorders (arthritis, inflammation, trauma) and dermatological issues through the advanced use of 3D/4D ULTRASOUND innovations. Trauma Diagnostics) Research / assessment of musculoskeletal disorders (arthritis, inflammation, trauma) and dermatological issues through the advanced use of 3D/4D ULTRASOUND innovations. Trauma Diagnostics) |
 TECH REVIEWER: Beta-testing, industry-wide comparative feature review/evaluation program. Drafting of FDA application / compliance documentation of digital imaging technologies (models, brands and generations) including sub-dermal and musculoskeletal treatment devices TECH REVIEWER: Beta-testing, industry-wide comparative feature review/evaluation program. Drafting of FDA application / compliance documentation of digital imaging technologies (models, brands and generations) including sub-dermal and musculoskeletal treatment devices |
 Internal study of all cancer issues and health disorders of victims associated with 9/11 and other disaster-related environmental toxic exposures. Collaboration with geological labs & environmental statistics. (See First Responders Cancer Resource) Internal study of all cancer issues and health disorders of victims associated with 9/11 and other disaster-related environmental toxic exposures. Collaboration with geological labs & environmental statistics. (See First Responders Cancer Resource) |
 Function review / performance evaluation program of all laser-based medical equipment including devices specializing in sub-dermal musculatory treatment of chronic disorders. Function review / performance evaluation program of all laser-based medical equipment including devices specializing in sub-dermal musculatory treatment of chronic disorders. |
|
Major Research PROJECTS • Efficacy of Injected Hyaluronidase Filler Reduction Dept Dermatology Mt Sinai • Photoacoustic and Optical Imaging • Doppler Evaluation of Radiation Treatment Response • 3D Doppler Sonography of Malignant Melanoma • 3D Imaging of Psoriasis • Doppler Vessel Density in Melanoma • Prostatic Volume Reduction Implementing Radiotherapy Treatment Application • Ultrasonography of the Spine in Rheumatoid Arthritis • Ultrasound Evaluation of the Patient with Rheumatoid Arthritis
|
Scientific PUBLICATIONS (see Pg. 6-19 books published & international presentations) |
|
Research Support and Fundraising EVENTS
 |
May 10, 2018- NYC; The LOTOS CLUB hosted the 2018 speaker series with Dr. Robert Bard's opening presentation on Early Detection & Prevention by NYCRA (New York Cancer Resource Alliance) and endorsed Dr. Bard to launch this theme because of his expanded knowledge in today's modern diagnostic technologies and non-invasive applications including the 4D Doppler ultrasound technology - much of which has been driven by European medical influence for the cancer treatment community. Dr. Bard is an internationally recognized leading expert in the use of this process for the screening, scanning and pre/post procedural monitoring of Breast, Prostate & Skin Cancers. He is also known for his public mission to replace surgical analysis of tumors with his coined "digital biopsies". Dr. Bard gave the standing-room only audience at the LOTOS CLUB an astounding look at the effectiveness of his imaging process to the surgical chain. He shared images of actual patient cases including the study of blood flow in tumors, behaviors of cysts, foreign bodies in trauma cases, fracture analysis and proven ways that cancers can be safely detected, studied and even treated with the use of non-surgical means. The high accuracy of 3D-4D Histogram analysis allows cancer treatment to be implemented without invasive biopsies that may spread tumor cells. (full article)